Chronic obstructive pulmonary disease (COPD) and metabolic fatty liver syndromes: a dangerous but neglected liaison
Abstract
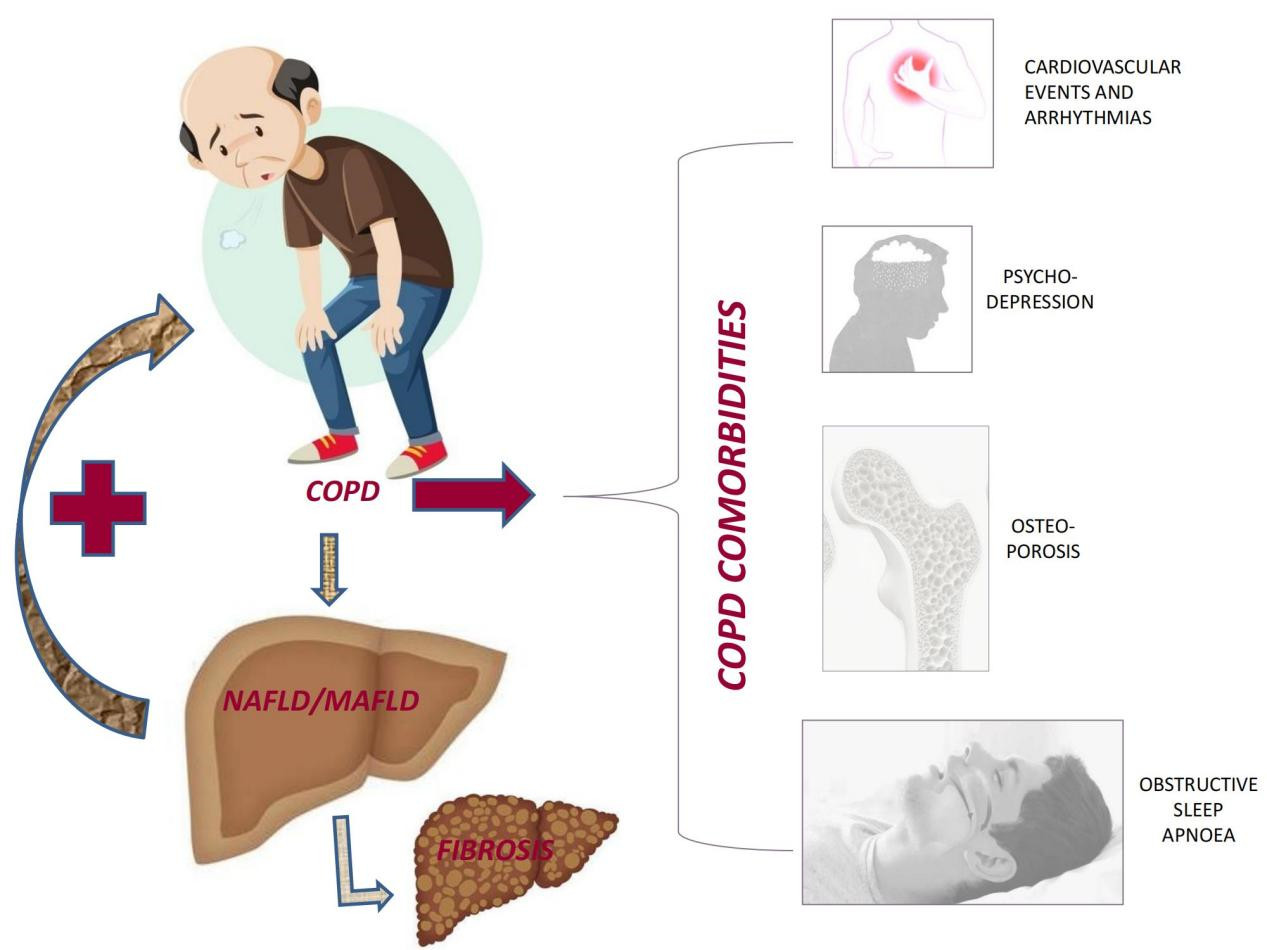
This perspective article aims at addressing the potential commonalities associated with chronic obstructive pulmonary disease (COPD) and the two metabolic fatty liver syndromes: nonalcoholic fatty liver disease (NAFLD) and metabolic (associated) fatty liver disease (MAFLD). To this end, we briefly review the definitions and burdens of COPD and NAFLD and highlight the differences in the diagnostic criteria of NAFLD and MAFLD. We also critically discuss the recent line of research trying to identify an association between COPD and NAFLD. Moreover, among the chief co-morbidities of COPD patients, we identify significant six that exert a major impact on the natural course of COPD: major cardiovascular events, cardiac arrhythmias, metabolic syndrome, obstructive sleep apnea, osteoporosis, and psychodepression. The potential role of NAFLD in each of these COPD co-morbidities is accurately examined based on published studies. We conclude that both COPD and NAFLD/MAFLD are heterogeneous systemic syndromes. While the complex mechanistic links underlying the association of NAFLD/MAFLD with COPD and its co-morbidities remain to be fully elucidated, we highlight that the diagnosis of metabolic fatty liver syndromes in patients with COPD might be clinically relevant, as it might allow identifying a subset of COPD individuals who, being at risk of severe clinical outcomes, would need more comprehensive treatment approaches.
Keywords
BACKGROUND
The commonalities and similarities shared by the lungs and the liver are impressive. These organs have a dual blood supply and serve similar physiological functions: antigen processing and regulation of energy homeostasis[1]. Chronic obstructive pulmonary disease (COPD) and fatty liver syndromes, [i.e., nonalcoholic fatty liver disease (NAFLD) and the more recently defined metabolic-associated fatty liver disease (MAFLD)], rather than discrete nosological entities, are best conceptualized as complex, chronic, systemic, and non-transmissible syndromes exhibiting a high grade of phenotypic variability and poorly predictable clinical courses[2,3].
Despite these commonalities and similarities, the clinical impact of the association of COPD and NAFLD/MAFLD is a relatively under-investigated arena: a PubMed Research of literature conducted on 21 January 2022 (NAFLD[Title/Abstract]) AND (COPD[Title/Abstract]) identified as few as 11 results (theses, cross-references, and other relevant references directly identified by the authors represent the basis of the present perspective article). Although the topic is understudied and probably underrated, we believe that both COPD and NAFLD/MAFLD are associated with systemic chronic inflammation and oxidative stress, with the ensuing risk of accelerated atherogenesis and cancer[1].
On these grounds, this perspective article discusses the evidence calling for more extensive research to ascertain the implications of co-morbid NAFLD/MAFLD among COPD individuals and vice versa.
COPD
COPD is characterized by chronic respiratory symptoms, particularly progressive exertional dyspnea, which in up to one-third of patients is associated with chronic cough and sputum[4]. According to guidelines, the diagnosis should be confirmed by the presence of poorly reversible airflow limitation, i.e., post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio < 0.7[4]. However, in clinical practice, and even in hospitalized patients, the diagnosis of COPD is mainly based on the presence of chronic respiratory symptoms and/or their exacerbations, smoking habits, age, or previous/ongoing treatment with COPD drugs, particularly inhaled long-acting bronchodilators and/or steroids, or their combination. COPD identifies a heterogeneous group of patients who, while sharing the common denominator of post-bronchodilator airflow limitation, also have variable phenotypical, pathological, and pathophysiological features[5]. Consistently, COPD has a complex natural history. This may start in early life and progress slowly, manifesting itself and being diagnosed and treated almost invariably after the age of 40, with cigarette smoking being the strongest risk factor for most subjects from industrialized countries[5]. Occupational, environmental, and indoor pollution are major risk factors, particularly in developing countries. Although a large variety of different established and emerging etiologic factors[6] embracing genetic determinants (e.g., α1-antitrypsin deficiency), exogenous (smoking, biomass fuels, occupational, or indoor pollutants), infective (viral, and bacterial), or endogenous factors (past infection of the lung, history of asthma and abnormal lung development, and abnormal inflammatory reaction of the airways) interacting throughout the life cycle, no etiological agent is found in a large fraction of spirometrically diagnosed COPD cases[5,7]. Additionally, owing to the large variety of concomitant chronic diseases, COPD should best be envisaged as a syndrome rather than a single disease entity[5,7] whose variable clinical phenotypes are prone to manifest different natural histories as a function of the variable comorbidity spectrum[7,8]. In particular, lung cancer and heart disease are the two most important co-morbidities associated with COPD mortality[9]. In agreement, COPD is considered the pulmonary chronic component of chronic multi-morbidity[4,10,11], as it is associated in > 90% of the patients[12] with at least one concomitant chronic disease mostly due to the same risk factors of all components of multi-morbidity, i.e., aging[13], smoking[4], alcohol consumption, physical inactivity[14], and/or early events, such as prematurity and low birth weight, respiratory infections, (e.g., respiratory syncytial virus), and asthma[15,16].
COPD is associated with high and increasing mortality globally[9] and has been projected to become one of the leading causes of mortality worldwide by 2021[4]. In Europe, the prevalence of COPD reportedly ranges between 4% and 10% in adults, with an expected increase of disease burden in the near future, mostly among older populations[4,17], and is one of the most frequent causes of hospitalization and in-hospital mortality[18].
The most common and best examined chronic COPD co-morbidities are cardiovascular (arterial hypertension, chronic heart failure, ischemic heart disease, cardiac arrhythmias[19,20], cerebrovascular disease[21]), obstructive sleep apnea (OSA)[22], osteoporosis[23], depression[24], metabolic syndrome (MetS) and its individual features (type 2 diabetes and obesity)[25,26], and lung cancer[27].
While the prevalence of individual co-morbidities widely varies across different populations[28], those listed above have been shown to have a direct impact on the clinical course of COPD. Indeed, in COPD, they are associated with an increased risk of exacerbations and hospitalizations[29,30], increased health care costs[31-33], as well as an increased risk of death[34-36]. Similar to the co-morbidities of all other chronic diseases, COPD co-morbidities are largely under-diagnosed and under-treated[37], unless actively searched for[12].
Chronic systemic inflammation, a common feature of most of the above co-morbidities, has been hypothesized to be a key factor linking COPD with its co-morbidities[38,39]. Interestingly, NAFLD/MAFLD, epidemiologically and clinically prevailing entities in the chronic liver disease (CLD) spectrum, are deemed to be strong risk factors for the future development of chronic cardio-metabolic diseases and other diseases, mainly because they are associated with low-grade chronic inflammation and increased oxidative stress[40,41].
CHRONIC LIVER DISEASES AND COPD
CLD is an etiologically, clinically, and histologically heterogeneous group of disorders spanning steatosis, steatohepatitis, chronic hepatitis, cirrhosis, and liver cancer. Collectively, CLD accounted for 287,000 deaths in Europe in 2019 (95%CI: 268,000-306,000), and 63,500 (58,916-67,530) of these were due to primary liver cancer[42]. These figures, compared to 1990, represent a 25% increase in all liver-related deaths and a 70% increase in deaths due to primary liver cancer[42]. Moreover, collectively, CLD ranks second only to ischemic heart disease as the leading cause of years of working life lost in Europe[42].
While the awareness that prevalence and incidence of the above-mentioned concomitant chronic diseases as well as of their important impact on the outcomes of COPD has increased over time[28], there are few published studies focusing on the relationship between liver diseases and COPD. The most striking - but not surprising - finding is that liver cirrhosis impacts on survival of patients with COPD[12]. However, the prevalence of liver cirrhosis among COPD patients is reportedly small[43], and the effect on pulmonary function is predictable considering the clinical manifestations of the disease[43]. Of concern, the most authoritative document on COPD[4], which highlights the importance of concomitant chronic diseases and has a separate chapter addressing co-morbidities, does not even mention liver diseases. This highlights the necessity to explore novel paradigms regarding the important role of hepatic conditions associated with COPD.
This apparent lack of interest from the pneumological field reflects our preliminary and incomplete understanding of the effect that most concurrent CLD cases have on respiratory function[43,44], except the portal hepatopulmonary hypertension syndrome and hepatopulmonary syndrome. However, in the last few years, Viglino et al. published pioneering papers on the relationship between COPD and NAFLD, the most common chronic liver disease in the general population globally, which has a major impact on morbidity and mortality[45-48].
In the first of their studies, they prospectively examined 111 adult patients with mild-to-severe COPD and, after excluding patients with cancer, significant alcohol consumption, and secondary causes of liver steatosis, assessed the prevalence and predictors of liver steatosis, nonalcoholic steatohepatitis (NASH), and fibrosis using Fibromax and a patented panel of three non-invasive serum biomarkers (SteatoTest for steatosis, NashTest for NASH, and FibroTest for fibrosis; BioPredictive SAS, Paris, France). Their data demonstrate that 41.4% of COPD patients had moderate to severe steatosis (as assessed by SteatoTest ≥ 0.57), 36.9% had borderline to definite NASH (NashTest > 0.25), and 61.3% had fibrosis stage ≥ F0-F1 (FibroTest ≥ 0.22), suggesting that progressive forms of NAFLD are significantly present in COPD[47]. Despite the limitations of the study design, as highlighted by one of us in the accompanying editorial[1], this was the first accurate estimate of the prevalence of NAFLD in COPD patients. In addition, the study described the metabolic abnormalities associated with NAFLD, confirming that NAFLD may indeed be a common co-morbidity in patients with COPD. Considering these results, the authors speculated that NAFLD might further increase the risk of future morbidity and mortality due to co-morbidities in COPD patients[47] and, therefore, should be searched for and possibly treated in patients with COPD and vice versa.
This recommendation was confirmed in a more recent intriguing post hoc analysis of one of the pillar studies in the field of COPD, the Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE)[49]. In their analysis, Viglino et al.[50] measured the density of the liver in the HRCT scans as a marker of liver steatosis. Liver density measured by computed tomography (CT) scan is an imaging proof of liver steatosis, with lower liver densities reflecting more fat infiltration and a liver density of 40 Hounsfield units (HU) corresponding to 30% fat accumulation. The relationship between this measurement and the Fibromax-based markers is unknown, and therefore a direct comparison of the prevalence of steatosis with previous studies could not be made. In addition, because parameters such as alcohol and liver enzymes were not collected in the ECLIPSE study, the results obtained with CT scan density measurement could not be used to assess the prevalence and role of NAFLD, NASH, and fibrosis.
Nonetheless, the study provided interesting results. While the prevalence of severe steatosis was not different between COPD patients (4.7%) and control “healthy smokers” and non-smokers (5.2%), in patients with COPD, the lowest liver density quartile compared to the highest liver density quartile was associated with coronary artery disease and stroke, after age and sex adjustment, suggesting that a low liver density (i.e., more severe steatosis) is a risk factor for cardiovascular co-morbidities in the COPD population[50]. This finding is in full agreement with a large body of NAFLD literature (such as discussed below). This specific study[50] may envisage a novel line of research in as much as CT scan assessed liver density may provide a unique opportunity to evaluate the degree of liver steatosis among the ever-increasing cohort of COPD patients who are undergoing HRCT-scan to better assess COPD (e.g., to characterize emphysema and patient candidacy to lung volume reduction surgery[51,52]), to evaluate other co-morbidities (e.g., coronary artery calcifications, pulmonary hypertension, and osteoporosis[53]), and for screening of lung cancer. This last objective is undoubtedly reinforced by the recent encouraging results[54] and the recommendations issued by the US Preventive Services Task Force[55]. This more liberal use of CT scans will provide pneumologists with a unique opportunity to conduct a systematic, non-invasive assessment of liver steatosis and its pathophysiological and clinical consequences among COPD patients. Similarly, retrospective analysis of large ongoing observational studies in smokers and COPD patients (e.g., COPDgene and SPIROMICS)[56,57] that include CT scan and several biomarkers might extend the pivotal observations of Vestbo et al.[49].
Considering that both COPD and MAFLD are risk factors for the future development of severe chronic diseases, hospitalizations, and premature mortality, we strongly believe that the co-existence of these two diseases is expected to identify a specific and novel cardio-metabolic “risky” COPD phenotype. Confirmation of our hypothesis would implicate an active search for and management of concomitant diseases through a holistic approach, even though the supporting evidence of its cost-benefit ratio is still elusive.
NAFLD CO-MORBIDITIES: EPIDEMIOLOGICAL ASSOCIATIONS
NAFLD defines a wide-ranging clinico-pathological spectrum of alcohol-like liver changes spanning from steatosis (i.e., intrahepatocyte fatty changes > 5%) to NASH (i.e., steatosis associated with cellular degeneration and variable amounts of inflammatory and fibrotic changes) to cirrhosis and hepatocellular carcinoma (HCC)[58]. By definition, these conditions are histologically identified in individuals who do not have any competing causes of (steatogenic) liver disease, notably including alcohol, and are mutually and bi-directionally associated with MetS and its individual features[59].
The average prevalence of NAFLD is 23.7% (95%CI: 16.1%-33.5%) of the general population in Europe, where it is rapidly becoming a leading cause of liver-related mortality and projected to become the leading cause of end-stage liver disease[42]. These impressive epidemiological figures exact high healthcare expenditures owing to direct and indirect costs across European countries and the USA[60].
Similar to COPD, NAFLD is a systemic syndrome rather than a single disease entity. This occurs due to the disease’s pathogenic, pathological, and clinical variability. For example, there are “genetic” and “metabolic” NAFLD types[61]; NAFLD is common in the obese, but also a “lean NAFLD” phenotype has been precisely characterized[62]. As regards the hepatic spectrum of disease, there is a variability of patho-mechanisms, and a variable susceptibility to disease progression over time, ranging from individuals with mild, stable disease to individuals with rapid fibrosis progression[63]. In addition, the mechanisms of development of HCC are incompletely understood[64]. Further to this hepatic spectrum of disease, some individuals will manifest principally extra-hepatic manifestations and complications of NAFLD, which span from cardio-metabolic to certain extra-hepatic cancer types[65-67].
Forty years after the term “NASH” was used for the first time, aimed at giving NAFLD a “positive” definition, namely by using the “metabolic” qualification as opposed to the “negative” nonalcoholic attribute, experts have recently proposed to rename NAFLD as MAFLD [i.e., metabolic (dysfunction) associated fatty liver disease]. Reception of the novel MAFLD nomenclature, although promptly endorsed by many, remains an ongoing process[68]. Compared to NAFLD, MAFLD is a shift in the paradigm, emphasizing the major causal role of metabolic dysfunction. Additionally, analysis of the common features shared by both NAFLD and MAFLD, together with the potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy of the newly defined MAFLD, as compared to NAFLD, suggests that, in the future, the broader MAFLD syndrome will likely be increasingly used as a standard to identify subjects at risk of progressive hepatic and extra-hepatic disease[40,69,70].
We firmly believe that the diagnosis of NAFLD/MAFLD in any given COPD patient has a potentially strong biological and clinical impact, given that NAFLD is a definite risk factor for the development of many of the above-described COPD cardiovascular co-morbidities. For example, tipping the balance in favor of a strong physiological impact of MAFLD on COPD course, Miao et al.[71], by evaluating as many as 2543 Chinese adults undergoing health check-up examinations, found that, after adjusting for confounding factors (age, sex, adiposity, smoking, and alcohol) and compared to those with NAFLD, individuals with MAFLD had a significantly lower predicted FVC (FVC: 88.27 ± 17.60% vs. 90.82 ± 16.85%, P < 0.05) and FEV1 (79.89 ± 17.34 vs. 83.02 ± 16.66%, P < 0.05). As expected, the most advanced MAFLD forms were associated with more severe spirometric findings such that, for each one-point increase in the non-invasive fibrosis biomarker FIB-4, FVC diminished by 0.507 [95% confidence interval (CI): -0.840 to -0.173, P < 0.003], and FEV by 0.439 (95%CI: -0.739 to -0.140, P < 0.004). Interestingly, statistical analysis conducted separately by sex yielded unchanged results[71].
To illustrate our thesis further, here we discuss NAFLD’s major role in modulating the risk of six among the most common and clinically relevant COPD co-morbidities: major cardiovascular events, cardiac arrhythmias, MetS, OSA, osteoporosis, and psychodepression. Collectively, these COPD systemic co-morbidities are major modifiers of both quality of life and reduced life expectancy among COPD patients, thus supporting the potential role of NAFLD in the clinical course of COPD patients.
Major cardiovascular events
A consistent line of research has identified NAFLD as a strong risk factor for fatal and non-fatal cardiovascular events. The best evidence for this was recently published by Mantovani et al.[65]. In their updated meta-analysis of 36 longitudinal studies (with a median 6.5-year follow-up) with aggregate data on 5,802,226 middle-aged individuals NAFLD (diagnosed histologically, with imaging techniques, or based on International Classification of Diseases (ICD) codes, in the absence of competing causes of steatosis, notably including alcohol either >20 g/day for either sex, or > 30 g/day for men and > 20 g/day for women) was associated with a moderately increased risk of fatal or non-fatal cardiovascular disease (CVD) events [pooled random-effects hazard ratio (HR): 1.45, 95%CI: 1.31-1.61; I² = 86.18%]. This risk markedly increased in parallel with the stage of liver fibrosis (pooled random-effects HR 2.50, 95%CI 1.68-3.72; I² = 73.84%), was independent of confounding factors (age, sex, adiposity measures, diabetes, and other common cardio-metabolic risk factors), and was not modified by sensitivity analyses. Given that the proportion of concurrent COPD among these NAFLD individuals is unknown, more studies are necessary to identify the additive risk on cardiovascular morbidity and mortality resulting from the association of both NAFLD and COPD in the same individuals.
Cardiac arrhythmias
Interestingly, NAFLD is also inherently associated with the risk of cardiomyopathy and cardiac arrhythmias - and particularly atrial fibrillation (AF)[72] - which are also common among COPD patients. Supporting this notion, Gong et al.[73], in their meta-analytic review of 19 published studies totaling 7,012,960 adult participants, found that NAFLD (diagnosed based on the ICD code, liver biopsy, imaging techniques, or fatty liver index in the absence of competing causes of CLD, notably including significant alcohol consumption) was independently associated with higher risks of AF [Odds ratios (OR): 1.71, 95%CI: 1.14-2.57; HR: 1.12, 95%CI: 1.11-1.13], prolonged QT interval (OR: 2.86, 95%CI: 1.64-4.99), premature atrial/ventricular contraction (OR: 2.53, 95%CI: 1.70-3.78), and heart block (OR 2.65, 95%CI: 1.88-3.72). Completing the spectrum of cardiovascular manifestations, NAFLD is reportedly associated with an increased risk of heart failure (HF) independent of confounding clinical and demographic factors. In agreement, Fudim et al.[74], retrospectively evaluating a cohort of Medicare beneficiaries, observed that, over a mean 14.3-month follow-up, patients with baseline NAFLD had a significantly higher risk of new-onset HF in adjusted analyses [adjusted HR (95%CI), 1.23 (1.18-1.29)], and the risk of HF was stronger for HF with preserved ejection fraction [adjusted HR (95%CI): 1.24 (1.14-1.34)] than with HF with reduced ejection fraction [adjusted HR (95%CI): 1.09 (0.98-1.2)]. Based on their comprehensive analysis of the published evidence, Mantovani et al.[75] recently concluded that “there is a strong association between NAFLD and increased risk of new-onset HF, regardless of the presence or absence of T2D and other co-existing cardiometabolic risk factors. The magnitude of this risk increases with the severity of liver disease in NAFLD (especially with higher fibrosis stage)”. Again, specific studies should prospectively evaluate the predicted unfavorable interaction of concurrent NAFLD and COPD in increasing the risk of HF.
Metabolic syndrome
The relationship between NAFLD and MetS is close, mutual, and bi-directional, as supported by several lines of evidence (reviewed in Ref.[59]). For example, Zhang et al.[76], using a simplified Bayesian network analysis constructed to infer the reciprocal causality, identified mutual associations between NAFLD (steatosis was diagnosed with ultrasonography) and MetS in a Chinese population. Based on a prospective large-scale health check-up database, they found that, in reciprocal causality, the effect of MetS on NAFLD was higher than that of NAFLD on MetS. This study, together with others, has led to the conclusion that NAFLD is more than “the hepatic manifestation of metabolic syndrome” but may also serve as the precursor of MetS[77-79]. Confirming this notion, a meta-analytic study conducted by Ballestri et al.[80] on 20 published studies found that NAFLD was associated with an increased risk of incident MetS over a median five-year follow-up period (range, 3-14.7 years) with a pooled relative risk of 1.80 (95%CI: 1.72-1.89). The risk varied based on the technique used to capture NAFLD ranging from 1.80 (95%CI: 1.72-1.89) for alanine aminotransferase (last vs. first quartile or quintile) to 3.22 (95%CI: 3.05-3.41) for ultrasonography. Intermediate values of risk were associated with NAFLD diagnosed with GGT [1.98 (95%CI: 1.89-2.07)[80]. The risk of progression from NAFLD at baseline to incident type 2 diabetes (T2D) in the medium term is also substantial. Mantovani et al.[66] conducted a meta-analysis of 33 studies totaling 501,022 individuals (30.8% with NAFLD), and, among these, 27,953 cases had incident diabetes over a median of five-year follow-up. This study has two findings: Firstly, NAFLD patients had a higher risk of incident diabetes (HR: 2.19, 95%CI: 1.93-2.48; I2 = 91.2%). Secondly, the risk of incident diabetes was higher among those with more “severe” NAFLD (HR: 2.69, 95%CI: 2.08-3.49; I2 = 69%) and also markedly increased across the severity of liver fibrosis stages (HR: 3.42, 95%CI: 2.29-5.11; I2 = 44.6%). Interestingly, all risks were independent of confounding factors (age, sex, adiposity measures. and other common metabolic risk factors), sensitivity analyses did not alter these findings, and no significant publication bias was disclosed[66]. These findings are clinically relevant given that both T2D and MetS are definite risk factors for the fibrotic progression of NAFLD and its transformation to HCC in a proportion of cases[81,82]. Specific studies should investigate the role, if any, of concurrent COPD in modulating this mutual association of progressive NAFLD forms with the MetS.
Obstructive sleep apnea
OSA describes repeated episodes of partial/total loss of respiratory airflow, which occur while sleeping and are associated with upper airway collapse in inspiration, strenuous breathing. And ominous cardio-metabolic consequences[83]. Musso et al.[84], by submitting 18 cross-sectional studies overall totaling 2183 participants to a meta-analytic review, showed that pooled ORs of OSA for the presence of NAFLD (diagnosed with histology, imaging, and altered liver enzymes) were 2.01 (95%CI: 1.36-2.97), 2.99 (1.79-4.99), 2.36 (1.46-3.82), and 2.60 (1.88-3.61), respectively. Pooled ORs of OSA for NASH, fibrosis-any stage, or advanced fibrosis in biopsy-proven NAFLD patients were 2.37 (1.59-3.51), 2.16 (1.45-3.20), and 2.30 (1.21-4.38), respectively. These findings remained unaltered after correction for confounding factors [age, sex, and body mass index (BMI)] indicating that OSA was associated with an increased risk of NAFLD, NASH, and hepatic fibrosis[84]. Although this study suggests that patients with OSA should best be screened for NAFLD and NASH, it fails to analyze the patho-mechanisms underlying these associations. Bringing these findings further, Sundaram et al., in a selected cohort of 36 adolescents with NAFLD and 14 lean controls, demonstrated that nocturnal hypoxia was a trigger for localized hepatic oxidative stress, an important factor associated with the progression of NASH and liver fibrosis in obese pediatric patients[85]. This study agrees with the finding that, in adults, OSA is indeed associated with NASH and advanced liver histology[86]. The evidence discussed above supports the notion that NAFLD forms with more advanced fibrosis are exposed to increased cardiovascular risk[65]. In this connection, OSA may trigger a vicious cycle leading to increased CVD risk via progressive liver fibrosis. Bettini et al.[87] cross-sectionally studied the relationships among OSA severity, steatosis extent in NAFLD, and cardiovascular risk in a cohort of 110 adult patients aged 18-65 years with OSA. The data show that the degree of steatosis in patients with NAFLD was significantly correlated with the severity of OSA, carotid intima-media thickness measurements, ICAM-1, and Lp(a), underscoring the need to screen for NAFLD in patients with OSA to ensure prompt risk stratification and intensive management approaches[87].
Osteoporosis
Although chronic inflammation, a definite feature of NAFLD, is a major risk factor for osteoporosis, and some studies have supported the association between low bone mineral density (BMD) and NAFLD, collectively, the data regarding this association are conflicting thus far. Upala et al.[88], therefore, conducted a meta-analytic review of eleven observational studies articles involving 1276 participants (638 with NAFLD) to ascertain the association between NAFLD and BMD in adults (≥ 18 years of age). These individuals had no other cause of liver disease, osteoporosis, or pathological bone disease at baseline. The main meta-analysis failed to demonstrate any significant difference in BMD between NAFLD patients and controls; of all variables analyzed, BMI had the strongest and most significant predictive effect on the difference in BMD[88]. Given that these authors concluded that further studies were required to fully show this relationship, Mantovani et al.[89] repeated a meta-analytic study in children or adolescents in whom NAFLD was diagnosed by either imaging or histology, and BMD Z-score was measured by dual-energy X-ray absorptiometry. Based on eight (observational cross-sectional or case-control) studies enrolling 632 children and adolescents (mean age, 12.8 years), 357 of whom had NAFLD; they were able to show significant differences in whole-body or lumbar BMD Z-scores between children/adolescents with and without NAFLD (n = 6 studies; pooled WMD: -0.48; 95%CI: 0.74 to -0.21; I2 = 55.5%), as well as between those with biopsy-proven NASH and those with no-NASH (n = 4 studies; pooled WMD: -0.27; 95%CI: -0.40 to -0.13; I2 = 0%). The aforementioned WMDs in BMD Z-scores were independent of confounding factors (age, sex, race/ethnicity, and BMI); findings were not modified by sensitivity analyses, and no evidence of significant publication bias was detected. These authors concluded that the presence and severity of NAFLD were significantly associated with reduced whole-body BMD Z-scores in children and adolescents[89]. However, given the observational design of the original studies submitted to a meta-analytic evaluation, causality remains unproven. Additionally, specific studies should be designed and conducted to explore the triangular association of reduced BMD, COPD, and NAFLD in adults.
Depression
The observation that poor diet, inadequate physical activity, and sedentary behavior are shared features of both NAFLD and psycho-depression[90] supports the rationale for conducting specific studies evaluating the association linking the latter to NAFLD in a proportion of cases. Gu et al., based on the analysis of seven published articles (most of which were cross-sectional), found that NAFLD patients had a significantly increased risk of depression (pooled OR = 1.13, 95%CI: 1.03-1.24, P = 0.007)[91]. Similarly, patients with depression also had a significantly increased risk of developing NAFLD (pooled OR = 1.46, 95%CI: 1.15-1.85, P = 0.002)[89]. Given the important clinical implications for the treatment of depression as both a cause and a consequence of NAFLD, this meta-analysis calls for prospective longitudinal studies to ascertain the cause-effect relationships. Moreover, COPD individuals with NAFLD are expected to be prone to an increased risk of depression, which remains to be ascertained with well-conducted prospective studies.
RESEARCH AGENDA
COPD and MetS are commonly associated in clinical studies, and patients are unaware of this double morbidity[92]. COPD and NAFLD/MAFLD are both complex syndromes with systemic manifestations whose co-morbidities extend far from the primarily affected organs, the lungs and liver, respectively. However, studies conducted on NAFLD patients have thus far neglected to define the proportion of patients who had concurrent COPD. From the side of COPD, which is often associated with cardio-metabolic co-morbidities, there is limited evidence to confirm/reject the notion that concurrent NAFLD carries, as it is logical to postulate, an increased risk of fatal and non-fatal cardiovascular events, HF, and metabolic complications. Of concern, chronic hypoxia and smoking, two definite pathophysiological features of COPD, both have the potential to trigger hepatic fibrogenesis, thereby promoting the development of progressive NAFLD forms[93]. These, in turn, are burdened with the highest risks of cardio-metabolic complications, therefore perpetuating a dangerous vicious cycle of progressive liver disease associated with COPD complications. Finally, the complex mechanistic links underlying the association of NAFLD, COPD, and its co-morbidities and complications must be fully elucidated. These include, among others, those molecular links associating NAFLD with accelerated atherogenesis and increased risk of cardiovascular disease such as systemic and hepatic metabolic derangements; intestinal dysbiosis; perturbed cellular and sub-cellular pathways; adipokines and pro-inflammatory cytokines; NAFLD-related liver inflammation, fibrosis and hepatocyte injury; and chronic hypoxia[94].
CONCLUSIONS
We critically discuss the grounds supporting the ominous and neglected association of COPD with metabolic fatty liver syndromes: our analysis calls for filling in research gaps. To accomplish these investigation priorities, we advocate more systematic collaboration between COPD physicians and NAFLD clinicians aimed at conducting systematic surveys exploring NAFLD features among those with COPD as well as COPD among NAFLD patients. In this regard, two elements of novelty are predicted to immensely facilitate such studies: the recent proposal to adopt the more descriptive MAFLD nomenclature (which, at variance with NAFLD, does not request liver biopsy or the exclusion of competing causes of steatosis)[40], together with the increased availability of liver imaging studies among COPD individuals submitted to CT scans in the setting of lung cancer screenings[55].
DECLARATIONS
Authors’ contributionsConceived the study design, performed bibliographic research and wrote the first drafts of the manuscript: Lonardo A, Beghe B, Fabbri L M
Revised the first drafts of the manuscript and addressed Reviewers’ comments: Lonardo A, Beghe B, Fabbri L M
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for PublicationNot applicable.
Copyright© The Author(s) 2022
REFERENCES
1. Lonardo A, Nascimbeni F, Ponz de Leon M. Nonalcoholic fatty liver disease and COPD: is it time to cross the diaphragm? Eur Respir J 2017;49:1700546.
3. Vanni E, Marengo A, Mezzabotta L, Bugianesi E. Systemic complications of nonalcoholic fatty liver disease: when the liver is not an innocent bystander. Semin Liver Dis 2015;35:236-49.
4. GOLD. 2022 Global initiative on Obstructive Pulmonary Disease (GOLD). Available from: www.goldcopd.org.
5. Lange P, Ahmed E, Lahmar ZM, Martinez FJ, Bourdin A. Natural history and mechanisms of COPD. Respirology 2021;26:298-321.
6. Zhang Y, Wang L, Mutlu GM, Cai H. More to explore: further definition of risk factors for COPD - differential gender difference, modest elevation in PM2.5, and e-cigarette use. Front Physiol 2021;12:669152.
7. Agustí A, Celli B. Natural history of COPD: gaps and opportunities. ERJ Open Res 2017;3:00117-2017.
8. Negewo NA, Gibson PG, McDonald VM. COPD and its comorbidities: impact, measurement and mechanisms. Respirology 2015;20:1160-71.
9. Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J 2006;28:1245-57.
10. Burke H, Wilkinson TMA. Unravelling the mechanisms driving multimorbidity in COPD to develop holistic approaches to patient-centred care. Eur Respir Rev 2021;30:210041.
11. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. The Lancet 2012;380:37-43.
12. Vanfleteren LE, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2013;187:728-35.
13. Divo MJ, Celli BR, Poblador-Plou B, et al. EpiChron - BODE collaborative group. chronic obstructive pulmonary disease (COPD) as a disease of early aging: evidence from the EpiChron Cohort. PLoS One 2018;13:e0193143.
14. Ng R, Sutradhar R, Yao Z, Wodchis WP, Rosella LC. Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J Epidemiol 2020;49:113-30.
15. Guerra S, Martinez FD. The complex beginnings of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2020;201:641-2.
16. Bush A. Impact of early life exposures on respiratory disease. Paediatr Respir Rev 2021;40:24-32.
18. Serra-Picamal X, Roman R, Escarrabill J, et al. Hospitalizations due to exacerbations of COPD: a big data perspective. Respir Med 2018;145:219-25.
19. Roversi S, Tonelli R, Fabbri LM. Breakthroughs in internal and respiratory medicine. The Lancet Respiratory Medicine 2015;3:600-2.
20. Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev 2018;27:180057.
21. Corlateanu A, Covantev S, Mathioudakis AG, et al. Chronic obstructive pulmonary disease and stroke. COPD 2018;15:405-13.
22. Voulgaris A, Archontogeorgis K, Pataka A, et al. Burden of Comorbidities in Patients with OSAS and COPD-OSAS Overlap Syndrome. Medicina (Kaunas) 2021;57:1201.
23. Bitar AN, Syed Sulaiman SA, Ali IAH, Khan I, Khan AH. Osteoporosis among patients with chronic obstructive pulmonary disease: systematic review and meta-analysis of prevalence, severity, and therapeutic outcomes. J Pharm Bioallied Sci 2019;11:310-20.
24. Zareifopoulos N, Bellou A, Spiropoulou A, Spiropoulos K. Prevalence, contribution to disease burden and management of comorbid depression and anxiety in chronic obstructive pulmonary disease: a narrative review. COPD 2019;16:406-17.
25. Staimez LR, Wei MY, Kim M, Narayan KMV, Saydah SH. Multimorbidity of four cardiometabolic and chronic pulmonary disease groups: prevalence and attributable fraction in US adults, 2007-2012. J Comorb 2017;7:22-32.
26. Kotlyarov S, Bulgakov A. Lipid metabolism disorders in the comorbid course of nonalcoholic fatty liver disease and chronic obstructive pulmonary disease. Cells 2021;10:2978.
27. Ang L, Ghosh P, Seow WJ. Association between previous lung diseases and lung cancer risk: a systematic review and meta-analysis. Carcinogenesis 2021;42:1461-74.
28. Divo M, Celli BR. Multimorbidity in patients with chronic obstructive pulmonary disease. Clin Chest Med 2020;41:405-19.
29. Feary JR, Rodrigues LC, Smith CJ, Hubbard RB, Gibson JE. Prevalence of major comorbidities in subjects with COPD and incidence of myocardial infarction and stroke: a comprehensive analysis using data from primary care. Thorax 2010;65:956-62.
30. MacLeod M, Papi A, Contoli M, et al. Chronic obstructive pulmonary disease exacerbation fundamentals: Diagnosis, treatment, prevention and disease impact. Respirology 2021;26:532-51.
31. Nielsen R, Johannessen A, Omenaas ER, et al. Excessive costs of COPD in ever-smokers. A longitudinal community study. Respir Med 2011;105:485-93.
32. Sharafkhaneh A, Petersen NJ, Yu HJ, et al. Burden of COPD in a government health care system: a retrospective observational study using data from the US veterans affairs population. Int J Chron Obstruct Pulmon Dis 2010;5:125-32.
33. Villegas C, Paz-Zulueta M, Herrero-Montes M, Parás-Bravo P, Madrazo Pérez M. Cost analysis of chronic obstructive pulmonary disease (COPD): a systematic review. Health Econ Rev 2021;11:31.
34. Miller J, Edwards LD, Agustí A, et al. Evaluation of COPD longitudinally to identify predictive surrogate endpoints (ECLIPSE) investigators. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med 2013;107:1376-84.
35. Chatila WM, Thomashow BM, Minai OA, Criner GJ, Make BJ. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:549-55.
36. Divo M, Cote C, de Torres JP, et al. BODE Collaborative Group. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012;186:155-61.
37. Fabbri LM, Luppi F, Beghé B, Rabe KF. Complex chronic comorbidities of COPD. Eur Respir J 2008;31:204-12.
39. Su B, Liu T, Fan H, et al. Inflammatory markers and the risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. PLoS One 2016;11:e0150586.
40. Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 2020;73:202-9.
41. Niederseer D, Wernly B, Aigner E, Stickel F, Datz C. NAFLD and cardiovascular diseases: epidemiological, mechanistic and therapeutic considerations. J Clin Med 2021;10:467.
42. Karlsen TH, Sheron N, Zelber-sagi S, et al. The EASL-Lancet Liver Commission: protecting the next generation of Europeans against liver disease complications and premature mortality. The Lancet 2022;399:61-116.
43. Rodriguez-Roisin R, Bartolome SD, Huchon G, Krowka MJ. Inflammatory bowel diseases, chronic liver diseases and the lung. Eur Respir J 2016;47:638-50.
44. Mantovani A, Lonardo A, Vinco G, et al. Association between non-alcoholic fatty liver disease and decreased lung function in adults: a systematic review and meta-analysis. Diabetes Metab 2019;45:536-44.
45. Kumar R, Priyadarshi RN, Anand U. Non-alcoholic fatty liver disease: growing burden, adverse outcomes and associations. J Clin Transl Hepatol 2020;8:76-86.
46. Mantovani A, Scorletti E, Mosca A, et al. Complications, morbidity and mortality of nonalcoholic fatty liver disease. Metabolism 2020;111S:154170.
47. Viglino D, Jullian-Desayes I, Minoves M, et al. Nonalcoholic fatty liver disease in chronic obstructive pulmonary disease. Eur Respir J 2017;49:1601923.
48. Viglino D, Plazanet A, Bailly S, et al. Impact of non-alcoholic fatty liver disease on long-term cardiovascular events and death in chronic obstructive pulmonary disease. Sci Rep 2018;8:16559.
49. Vestbo J, Anderson W, Coxson HO, et al. ECLIPSE investigators. Evaluation of COPD longitudinally to identify predictive surrogate end-points (ECLIPSE). Eur Respir J 2008;31:869-73.
50. Viglino D, Martin M, Almeras N, et al. Evaluation of COPD longitudinally to identify predictive surrogate endpoints (ECLIPSE) investigators. Low liver density is linked to cardiovascular comorbidity in COPD: an ECLIPSE cohort analysis. Int J Chron Obstruct Pulmon Dis 2019;14:3053-61.
51. Hartman JE, Criner GJ, Moore WH, et al. HRCT characteristics of severe emphysema patients: Interobserver variability among expert readers and comparison with quantitative software. Eur J Radiol 2021;136:109561.
52. Klooster K, Valipour A, Marquette CH, et al. Endobronchial coil system versus standard-of-care medical management in the treatment of subjects with severe emphysema. Respiration 2021;100:804-10.
53. Singhvi D, Bon J. CT imaging and comorbidities in COPD: beyond lung cancer screening. Chest 2021;159:147-53.
54. de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume ct screening in a randomized trial. N Engl J Med 2020;382:503-13.
55. Toumazis I, de Nijs K, Cao P, et al. Cost-effectiveness evaluation of the 2021 US preventive services task force recommendation for lung cancer screening. JAMA Oncol 2021;7:1833-42.
56. Regan EA, Hokanson JE, Murphy JR, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD 2010;7:32-43.
57. Couper D, LaVange LM, Han M, et al. SPIROMICS Research Group. Design of the subpopulations and intermediate outcomes in COPD study (SPIROMICS). Thorax 2014;69:491-4.
59. Lonardo A, Leoni S, Alswat KA, Fouad Y. History of nonalcoholic fatty liver disease. Int J Mol Sci 2020;21:5888.
60. O'Hara J, Finnegan A, Dhillon H, et al. Cost of non-alcoholic steatohepatitis in Europe and the USA: The GAIN study. JHEP Rep 2020;2:100142.
61. Luukkonen PK, Qadri S, Ahlholm N, et al. Distinct contributions of metabolic dysfunction and genetic risk factors in the pathogenesis of non-alcoholic fatty liver disease. J Hepatol 2022;76:526-35.
62. Chen F, Esmaili S, Rogers GB, et al. Lean NAFLD: a distinct entity shaped by differential metabolic adaptation. Hepatology 2020;71:1213-27.
63. Arrese M, Arab JP, Barrera F, et al. Insights into nonalcoholic fatty-liver disease heterogeneity. Semin Liver Dis 2021;41:421-34.
64. Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med 2018;24:908-22.
65. Mantovani A, Csermely A, Petracca G, et al. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology 2021;6:903-13.
66. Mantovani A, Petracca G, Beatrice G, et al. Non-alcoholic fatty liver disease and risk of incident diabetes mellitus: an updated meta-analysis of 501 022 adult individuals. Gut 2021;70:962-9.
67. Mantovani A, Petracca G, Beatrice G, et al. Non-alcoholic fatty liver disease and increased risk of incident extrahepatic cancers: a meta-analysis of observational cohort studies. Gut 2022;71:778-88.
68. Lonardo A. Renaming NAFLD to MAFLD: could the lde system assist in this transition? J Clin Med 2021;10:492.
69. Xian YX, Weng JP, Xu F. MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy. Chin Med J (Engl) 2020;134:8-19.
70. Polyzos SA, Kang ES, Tsochatzis EA, et al. Commentary: nonalcoholic or metabolic dysfunction-associated fatty liver disease? Metabolism 2020;113:154413.
71. Miao L, Yang L, Guo L, et al. Metabolic dysfunction-associated fatty liver disease is associated with greater impairment of lung function than nonalcoholic fatty liver disease. Journal of Clinical and Translational Hepatology 2022;000:000-000.
72. Anstee QM, Mantovani A, Tilg H, Targher G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol 2018;15:425-39.
73. Gong H, Liu X, Cheng F. Relationship between non-alcoholic fatty liver disease and cardiac arrhythmia: a systematic review and meta-analysis. J Int Med Res 2021;49:3000605211047074.
74. Fudim M, Zhong L, Patel KV, et al. Nonalcoholic fatty liver disease and risk of heart failure among medicare beneficiaries. J Am Heart Assoc 2021;10:e021654.
75. Mantovani A, Byrne CD, Benfari G, et al. Risk of heart failure in patients with nonalcoholic fatty liver disease: JACC review topic of the week. J Am Coll Cardiol 2022;79:180-91.
76. Zhang Y, Zhang T, Zhang C, et al. Identification of reciprocal causality between non-alcoholic fatty liver disease and metabolic syndrome by a simplified Bayesian network in a Chinese population. BMJ Open 2015;5:e008204.
77. Lonardo A, Ballestri S, Marchesini G, Angulo P, Loria P. Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis 2015;47:181-90.
78. Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease (NAFLD): updates and future directions. Dig Liver Dis 2017;49:471-83.
79. Lonardo A, Nascimbeni F, Mantovani A, Targher G. Hypertension, diabetes, atherosclerosis and NASH: cause or consequence? J Hepatol 2018;68:335-52.
80. Ballestri S, Zona S, Targher G, et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 2016;31:936-44.
81. Pang Y, Kartsonaki C, Turnbull I, et al. Diabetes, plasma glucose, and incidence of fatty liver, cirrhosis, and liver cancer: a prospective study of 0.5 million people. Hepatology 2018;68:1308-18.
82. Nasr P, Blomdahl J, Kechagias S, Ekstedt M. Modifiers of liver-related manifestation in the course of NAFLD. Curr Pharm Des 2020;26:1062-78.
83. Destors M, Tamisier R, Galerneau LM, Lévy P, Pepin JL. [Pathophysiology of obstructive sleep apnea syndrome and its cardiometabolic consequences]. Presse Med 2017;46:395-403.
84. Musso G, Cassader M, Olivetti C, et al. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. a systematic review and meta-analysis. Obes Rev 2013;14:417-31.
85. Sundaram SS, Halbower A, Pan Z, et al. Nocturnal hypoxia-induced oxidative stress promotes progression of pediatric non-alcoholic fatty liver disease. J Hepatol 2016;65:560-9.
86. Corey KE, Misdraji J, Gelrud L, et al. Obstructive sleep apnea is associated with nonalcoholic steatohepatitis and advanced liver histology. Dig Dis Sci 2015;60:2523-8.
87. Bettini S, Serra R, Fabris R, et al. Association of obstructive sleep apnea with non-alcoholic fatty liver disease in patients with obesity: an observational study. Eat Weight Disord 2022;27:335-43.
88. Upala S, Jaruvongvanich V, Wijarnpreecha K, Sanguankeo A. Nonalcoholic fatty liver disease and osteoporosis: a systematic review and meta-analysis. J Bone Miner Metab 2017;35:685-93.
89. Mantovani A, Gatti D, Zoppini G, et al. Association between nonalcoholic fatty liver disease and reduced bone mineral density in children: a meta-analysis. Hepatology 2019;70:812-23.
90. Lonardo A, Ballestri S. Perspectives of nonalcoholic fatty liver disease research: a personal point of view. Explor of Med ;2020:1:[Online First].
91. Gu Y, Zhang W, Hu Y, Chen Y, Shi J. Association between nonalcoholic fatty liver disease and depression: a systematic review and meta-analysis of observational studies. J Affect Disord 2022;301:8-13.
92. Piazzolla G, Castrovilli A, Liotino V, et al. Metabolic syndrome and chronic obstructive pulmonary disease (COPD): the interplay among smoking, insulin resistance and vitamin D. PLoS One 2017;12:e0186708.
93. Rosato V, Masarone M, Dallio M, et al. NAFLD and extra-hepatic comorbidities: current evidence on a multi-organ metabolic syndrome. Int J Environ Res Public Health 2019;16:3415.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Lonardo A, Beghe B, Fabbri LM. Chronic obstructive pulmonary disease (COPD) and metabolic fatty liver syndromes: a dangerous but neglected liaison. Metab Target Organ Damage 2022;2:6. http://dx.doi.org/10.20517/mtod.2022.06
AMA Style
Lonardo A, Beghe B, Fabbri LM. Chronic obstructive pulmonary disease (COPD) and metabolic fatty liver syndromes: a dangerous but neglected liaison. Metabolism and Target Organ Damage. 2022; 2(2): 6. http://dx.doi.org/10.20517/mtod.2022.06
Chicago/Turabian Style
Lonardo, Amedeo, Bianca Beghe, Leonardo Michele Fabbri. 2022. "Chronic obstructive pulmonary disease (COPD) and metabolic fatty liver syndromes: a dangerous but neglected liaison" Metabolism and Target Organ Damage. 2, no.2: 6. http://dx.doi.org/10.20517/mtod.2022.06
ACS Style
Lonardo, A.; Beghe B.; Fabbri LM. Chronic obstructive pulmonary disease (COPD) and metabolic fatty liver syndromes: a dangerous but neglected liaison. Metab Target Organ Damage. 2022, 2, 6. http://dx.doi.org/10.20517/mtod.2022.06
About This Article
Copyright
Data & Comments
Data
 Cite This Article 25 clicks
Cite This Article 25 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.